Skin Problems
Skin problems are conditions that affect your skin. They may cause rashes, inflammation, itchiness or other changes. Some conditions may be genetic, while lifestyle factors may cause others. It’s treatment may include medications, creams or ointments, or lifestyle changes.
Importance of Skin
Not only does the skin hold everything in, it also plays a crucial role in providing an airtight, watertight and flexible barrier between the outside world and the highly regulated systems within the body to stay away from various skin problems. It also helps with temperature regulation, immune defence, vitamin production, and sensation.
Our skin is a big deal – literally. It’s the largest organ in the body and one of the most complicated. It has many roles in the maintenance of life and health, but also has many potential skin problems, with more than 3,000 possible skin disorders.
The skin is unique in many ways, but no other organ demands so much attention and concern in both states of disease and health. There is a huge focus on skin health, with fierce competition to have glowing, clearer, healthier, younger and fresher skin. And this focus can cause secondary problems with self-esteem and mental health.
The structure of the skin
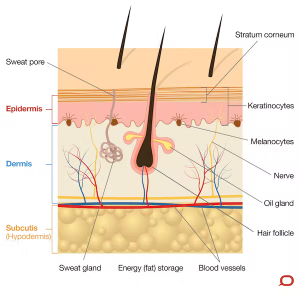
The skin is divided into three layers known as the epidermis, dermis and subcutis. These layers are well defined but together they allow the skin to function effectively.
The epidermis is the outermost, cellular layer of the skin which varies in thickness depending on the body site. On average it’s less than half a millimetre thick. The epidermis resembles a “brick wall” of cells known as keratinocytes, which are bound tightly together and act to prevent free movement of moisture, pathogens and chemicals into or out of the body.
Keratinocytes replicate from the basal layer and work their way up to the outer surface (known as the stratum corneum) over a period of about 28 days. Once they reach the surface the tight bonds between them break apart and they are shed.
Other than keratinocytes, pigment-producing cells known as melanocytes and immune cells known as Langerhans cells also exist within the epidermis. Melanocytes inhabit the basement membrane, at the base of the epidermis and produce a pigment known as melanin both innately (giving the skin its natural colour), and in response to ultraviolet light (UV) exposure (giving the skin a sun tan).
The melanin is a brown pigment that is taken up into the overlying keratinocytes. This pigment will then absorb UV light (from the sun) when it hits the skin, thereby protecting the basal calls underneath from UV damage.
The epidermal cells also develop hair follicles, sweat glands and sebaceous (oil) glands which extend down into the layer below known as the dermis. The small ducts from each of these glands open onto the skin surface. Sweat and sebum (oil) provide an antibacterial and protective barrier on the skin.
The dermis lies beneath the epidermis and is 20-30 times thicker. It’s made up of a dense layer of fibrous (collagen) and elastic (elastin) tissue. The dermis gives the skin its integrity, strength and elasticity; and houses blood vessels, glands and hair follicles, as well as nerves and their receptors.
Beneath the dermis lies the subcutis (also known as the hypodermis), a specialised layer of adipose (fat) and fibrous tissue. The thickness of this layer varies dramatically depending on the site and a person’s body shape and weight. It cushions the body from external trauma, insulates from the cold and stores energy (fat).
The function of the skin in avoiding skin problems
The extraordinary array of functions performed by healthy skin is still coming to light. The basic day-to-day functions include:
- Working as a barrier – protecting against water loss as well as physical and chemical injury, and bugs
- Helping us fight off bugs, allergens, toxins and carcinogens via the parts of our immune system that exist in our skin
- Regulating our temperature by dilating and constricting our blood vessels near the skin surface, controlling the transfer of heat out of the body. Temperature is also regulated by evaporative cooling due to sweat production and by the insulating effect of erect hairs on the skin surface.
- Heat loss is also affected by the insulating layer of subcutaneous fatProtecting us from UV radiation by producing melanin
- Giving us the sense of touch _ providing interaction with physical surroundings, allowing all fine and gross motor activities and allowing pleasurable and sexual stimulation
- The production of Vitamin D, which helps prevent many skin problems including osteoporosis, cancer, heart disease, obesity and neurological diseases
- Wound healing, Beauty and physical attraction – the quality and condition of the skin greatly contributes to the perception of health, wellness, youth and beauty.
Types of Skin Problems
Although most skin problems affecting the skin originate in the layers of the skin, such abnormalities are also important factors in the diagnosis of a variety of internal diseases. There is some truth in the belief that the skin mirrors a person’s internal health. Often, the visibility and accessibility of skin make it the first organ of the body to show detectable signs of underlying disease. Abnormalities of the skin frequently suggest metabolic, malignant, and glandular diseases.
Like other tissues, skin is afflicted by all types of pathological changes, including hereditary, inflammatory, benign and malignant (neoplastic), endocrine, hormonal, traumatic, and degenerative processes. Emotions affect the health of the skin as well. The reaction of the skin to these diseases and disorders differs from that of other tissues in many ways.
For example, extensive inflammation of the skin may affect metabolism within other organs and systems of the body, causing anemia, circulatory collapse, disorders of body temperature, and disturbance of water and electrolyte balance in the blood. The skin has such vigorous healing properties, however, that widespread injury, as in thermal burns, may be followed by a marked degree of regrowth of the injured or diseased areas, with a disproportionally small degree of scarring.
Types
Some skin problems are minor. Others cause severe symptoms. Some of the most common diseases include:
- Acne, blocked follicles that lead to oil, bacteria and dead skin buildup in your pores.
- Alopecia areata, losing your hair in small patches.
- Atopic dermatitis (eczema), dry, itching that leads to swelling, cracking or scaliness.
- Psoriasis, scaly skin that may swell or feel hot.
- Raynaud’s phenomenon, periodic reduced blood flow to your fingers, toes or other body parts, causing numbness or color change.
- Rosacea, flushed, thick skin and pimples, usually on the face.
- Cancer, uncontrolled growth of abnormal skin cells.
- Vitiligo, patches that lose pigment.
Certain lifestyle factors can lead to the development of skin problems. Underlying causes may affect your skin, too. Common causes of skin problems include:
- Bacteria trapped in your pores or hair follicles.
- Conditions that affect your thyroid, kidneys or immune system.
- Contact with environmental triggers, such as allergens or another person’s skin.
- Genetics.
- Fungus or parasites living on your skin.
- Medications, such as the ones that treat inflammatory bowel disease (IBD).
- Viruses.
- Diabetes.
- Sun.
These problems symptoms vary significantly, depending on what condition you have. The changes are not always due to their problems.
For example, you may get a blister from wearing ill-fitting shoes. However, when changes show up with no known cause, they may be linked to an underlying condition.
Hereditary skin problems
The formation of almost all components of the skin (for example, hair texture and colour and skin pigmentation and thickness) is under genetic control. A large number of common skin problems also are directly or indirectly determined by a person’s genotype (genetic constitution), but their expression may require an external influence or an altered hormonal milieu.
The hereditary skin problems psoriasis and atopic eczema are examples of skin disorders in which sunlight (as an extrinsic factor) or stress (as an intrinsic factor) activate the condition. Even when heredity has an immediate determining role, other factors may influence the expression of disease. The hereditary blood vessel diseases of the skin, for example, many of which are under direct genetic control, sometimes do not become evident until the hormonal changes of puberty create conditions optimal for disease expression.
A common genetic abnormality is the nevus, often called a mole or birthmark. Nevi are due to primary abnormalities in the structure or number of skin cells. A local increase in the concentration of melanocytes is termed a melanocytic or pigmented nevus; an area of increased capillary concentration, a capillary nevus. In nevus anemicus, an area of skin is pale because of reduced blood flow, even though there is no evidence of a structural disorder. Although most nevi are benign, malignant transformation may cause melanocytic nevi.
If an abnormality is inherited as an autosomal dominant trait and one parent is affected, then, from the laws of Mendelian inheritance, each child has a 50 percent risk for the disease. Amniocentesis, often performed between the 12th and 20th weeks of pregnancy, entails little risk to the mother or fetus and makes it possible to diagnose prenatally severe disorders such as epidermolysis bullosa, a blistering and scarring disorder; albinism, or a generalized lack of pigment from the skin; and xeroderma pigmentosum, a precancerous condition in which sunlight-induced skin damage cannot be enzymatically corrected by the affected skin cells.
Causes of Skin Problems
Generally, the skin problems may cause:
- Discolored patches (abnormal pigmentation).
- Dry skin.
- Open sores, lesions or ulcers.
- Peeling skin.
- Rashes, possibly with itchiness or pain.
- Red, white or pus-filled bumps.
- Scaly or rough.
Some health conditions can increase your chances of developing a disease. You may be more likely to experience changes or symptoms if you have:
- Diabetes: People with diabetes may have trouble with wound healing, particularly on their feet.
- Inflammatory bowel disease (IBD): Some IBD medications can lead to problems such as vitiligo or eczema.
- Lupus: This chronic condition can lead to inflammation and skin problems, such as rashes, sores or scaly patches.
Changes can also be the result of pregnancy, stress or hormonal changes. For example, melasma is one of the common skin problems that mostly affects pregnant women.
Conditions like alopecia areata, acne, Raynaud’s phenomenon or rosacea may get worse when you’re stressed.

Skin problems caused by cosmetics
We use cosmetics to make ourselves look better, but sometimes a make-up allergy can cause some unsightly skin conditions instead.
Irritant Cosmetic Dermatitis
Signs and Symptoms of Irritant Cosmetic Dermatitis
The patient may experience only a burning or stinging sensation after applying the cosmetic on the skin, but in severe cases, itchiness, redness, swelling and later scaling and peeling of the skin can occur.
Treatment of Irritant Cosmetic Dermatitis
Allergic Contact Dermatitis
Another important disease in this segment of skin problems caused by cosmetics is allergic contact dermatitis, which occurs less frequently than irritant contact dermatitis. It is often difficult to differentiate between the two by the appearance of the rash alone. Cosmetics ingredients that can cause skin allergy include fragrances, preservatives and sunscreens.
Symptoms and Signs of Allergic Contact Dermatitis
Treatment of Allergic Contact Dermatitis
Cosmetics induced pimples
Special Cosmetic Allergies
Hair-dye allergy is one of the most common causes of cosmetic dermatitis in men and women. Some people are able to dye their hair initially without any problem, but may suddenly develop an allergy to the dye after repeated use. The face, ears and neck are often affected.
Know More about Skin Problems
Visit our treatments page to know more about your exact skin problem to help you consult the right doctor.
Consult
Consult one of our vaidyas to speak about your skin problems and find solutions to them. Take an appointment from the vaidya of your choice, at the day and time of your choice, and even the language of your choice.